Are you diagnosed with HSV2 and planning to delay plastic surgery due to the HSV-2 breakout? What are the symptoms of HSV 2, and can you get plastic surgery with HSV2? We’ve got you covered; read this article till the end.
Not everyone who has HSV-2 exhibits symptoms or even knows they are infected. According to research, 87% of HSV-2 carriers under 50 have never had a diagnosis. Most are undiagnosed or have fragile symptoms that can be confused for other skin disorders.
What is HSV-2?
Herpes virus Type 2 (HSV-2) is a related virus that can also cause facial herpes, but it most often causes genital herpes. Type 2 herpes is a more severe form, which is most often received during unprotected or protected sexual intercourse. When an individual is infected with the herpes virus, it will remain in their body.
Facts vs Common Myths About Herpes:
Because herpes is a virus that spreads from person to person, there are many herpes myths floating around the internet.
While some appear to persist despite being completely false, others are based on incorrect facts. There are numerous myths, rumours, and half-truths about herpes, such as the misconception that infection with the virus prevents one from ever having sex again and that it is a rare, unusual disease. Underneath, we’ve recorded the most recognized legends about herpes and given logical information to restate any misinformation.
Myth 1: Symptoms are inevitable if you have herpes.
This is one of the most well-known herpes legends — that assuming you’re tainted; you will have side effects of the infection. Herpes does not always cause symptoms. Only about one in five people with herpes will exhibit visible symptoms like oral cold sores or genital herpes lesions.
Most people with herpes don’t know they have it because the virus doesn’t show signs in most people and stays dormant. That does not mean that you cannot look for visible herpes symptoms. In our HSV-1 vs HSV-2 guide, you’ll learn about all the symptoms you might experience before a herpes outbreak and what you can look for in someone else to see if they’re a carrier.
Myth 2: Only your mouth and genitals are affected by HSV-1 and HSV-2.
Another common misconception is that HSV-1, the most prevalent type of herpes, only causes cold sores around the mouth and gums, while HSV-2, the less general type, only ever causes genital sores.
Like many other myths, this is based on the fact that HSV-1 and HSV-2 affect different body parts. Even if you have HSV-1, you can still transmit genital herpes to another person through physical contact, so oral sex might be enough to spread the virus.
Additionally, oral contact, such as a kiss, can spread HSV-1. In contrast, HSV-2 spreads only through sexual contact. However, oral transmission of HSV-2 is also possible but uncommon.
Myth 3: Herbs, vitamins, and other natural remedies can treat herpes.
Sadly, HSV-1 and HSV-2 are viral infections that last a lifetime and have no known treatment. However, antiviral medications like valacyclovir, which help control outbreaks and reduce the risk of HSV-2 and HSV-1 transmission, can treat both types of herpes.
Naturally, this has not stopped the alternative medicine industry from offering a variety of “all-natural” herpes remedies and vitamins, including herbal blends of garlic and echinacea, lemon balm, and various natural extracts.
Even though some of these products may temporarily alleviate the physical discomfort caused by cold sores and herpes lesions (though none are as effective as medication for herpes), none of these alternative treatments will eradicate herpes.
Myth 4: Herpes is a single virus.
Herpes simplex infection (HSV), such as HSV-1 or HSV-2 to other types of herpes, such as herpes zoster (shingles), all fall under the umbrella term “herpes.”
The herpes virus behaves to each kind, sleeping off in a different part of your body between outbreaks. The most common variant of herpes, HSV-1 (herpes simplex 1), affects approximately half of all adults, or 65% of people between the ages of 14 and 49 worldwide, according to the World Health Organization.
Let us be clear for the record: There is currently no treatment for herpes. You never lose it once you have it.
What does HSV-2 look like?
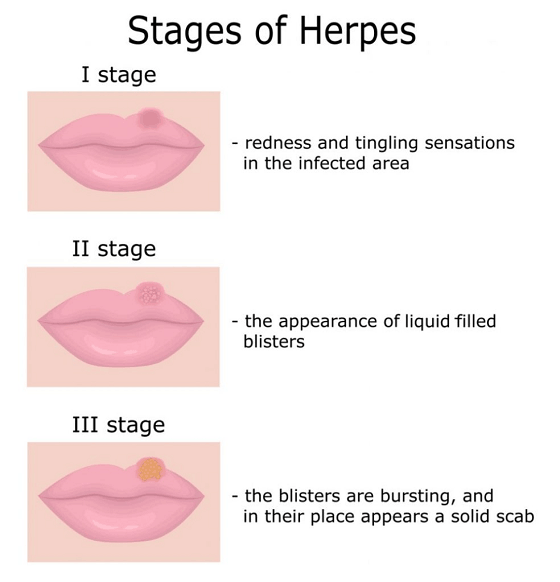
When a disease is about to happen, people experience prodromal (precursor) symptoms like itching, tingling, or burning near the area where the sores might appear.
Shortly after, a cluster of itchy or painful blisters filled with fluid will appear on the vagina. Genital herpes symptoms can vary from person to person. It causes a massive outbreak in some people and an uncomfortable rash or redness. It can be mistaken for other conditions. Both the size and density of the blisters might vary. The blisters become open sores that may bleed or exude a yellowish substance when they start to rupture.
SYMPTOMS

When symptoms appear, they involve the sudden emergence of tiny blisters near the genitalia or rectum. The blisters will soon burst, leaving severe ulcers that flow, crust over, and heal in two to four weeks.
You may also experience the following signs and symptoms:
- Blisters on the lips or inside the mouth
- Fever, headache, or joint pain
- difficulty urinating.
TRIGGERS
Following a person’s first outbreak, the virus travels through nerve pathways to the central nervous system and stays dormant. Factors that trigger a flurry of new fever blisters include stress, illness, fever, sun exposure, injuries, or surgery.
Genital herpes symptoms disappear only to return as recurrent outbreaks. The first outbreak, which can last two to three weeks, is the worst for most people. Future flare-ups get better and last less time. Some people shed the infection.
The following factors may increase the likelihood of outbreaks:
- Bacterial or viral infections
- Menstrual cycles
- Stress
The likelihood of developing recurrent genital herpes increases in the first year following the initial infection and then declines.
Plastic surgery may cause stress in you which might worsen your HSV-2 .Hence, No such question arises if can you get plastic surgery with HSV-2.
HOW DO DERMATOLOGISTS TREAT HERPES
HSV-2 has no treatment. The good news is that sores heal on their own. Because treatment can alleviate symptoms and reduce the duration of an outbreak, many people choose to treat herpes genitals. An over-the-counter antiviral cream or ointment, for instance, may alleviate symptoms of cold sores.
The following prescription antiviral medications have been granted FDA approval for treating both types of herpes simplex:
- Valacyclovir
- Acyclovir,
- Famciclovir
These are effective treatments for herpes. These treatments, when taken every day, can shorten the duration of an oral or genital herpes outbreak as well as reduce the severity and frequency of attacks. They can also assist in stopping infected individuals from spreading the virus.
HSV-2 infection has been proven to be associated with a three-fold risk of HIV acquisition.
You can consult your dermatologist asking her about can you get plastic surgery with HSV-2.
Complications in HSV-2
Those with HIV and HSV-2 disease are more prone to send HIV to others. HSV-2 infection is one of the most frequent infections in people with HIV.
You increase your chance of HIV Transmission if you have genital herpes and engage in sexual activity; when you have blisters (human immunodeficiency virus)ned, they will go away if the condition has returned.
HSV-2 can cause meningoencephalitis, a brain infection, and widespread infection.
Plastic Surgery
Cosmetic surgery can alter your body to treat physical ailments or improve beauty. Your face, neck, breasts, stomach, arms, and legs may be the subject of surgical treatments. Surgery for reconstruction restores function by repairing flaws or wounds. Cosmetic surgery improves for non-medical purposes.
Can you get plastic surgery with HSV-2?
There is NO justification for operating on you while you have an active infection in the location where the surgery is being performed. That would involve accepting unnecessary risks that wouldn’t exist if we postponed the surgery till the treatment was completed.
Stress triggers HSV-2; plastic surgery may also be a source of distress as it’s not easy to go through such a risky procedure.
So the answer to your question ” can you get plastic surgery with HSV-2″ is an obvious NO!
You should also check with your plastic surgeon, telling him your history of HSV-2.
Conclusion
Therefore revising the content as mentioned earlier, Herpes genital’s is a transmitted illness (STD). Anyone who engages in sexual activity can contract this virus, which is caused by genital herpes. Many infected individuals never have symptoms, thus unaware that they are infected. They never develop painful sores; if they do, the outbreaks are usually severe in the first year. Four or more outbreaks may occur in a year for certain persons. The outbreaks lessen in frequency over time. If your spouse doesn’t have genital sores, you should avoid having sex both while you have them and for a few days after they clear up if you do. You might infect your partner with herpes when you have sores.
You increase your chance of HIV Transmission if you have genital herpes and engage in sexual activity when you have blisters (human immunodeficiency virus). Through a herpes sore, this virus can enter your body.
So, If you have genital herpes, yeast infection outbreak, or any other illness, it is highly recommended that you wait until the infection has resolved before undergoing any vaginal procedure. Hopefully, now you’re aware if can you get plastic surgery with HSV-2 or not.









